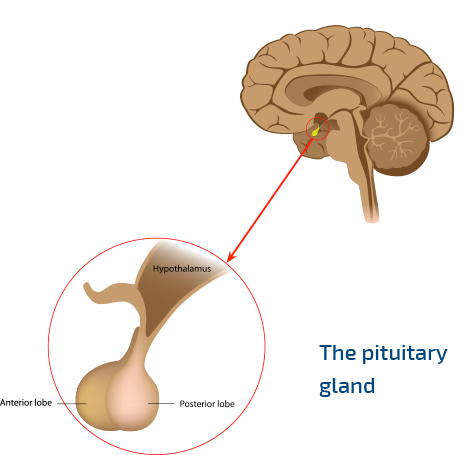
What is growth hormone deficiency?
When the pituitary gland doesn’t make enough growth hormone – or, in some cases, doesn’t make any at all – this condition is called growth hormone deficiency, or GHD. Scientists are still learning more about the causes of GHD. Patients may have GHD from childhood, or it may occur when they are adults, due to factors including head injuries or a type of pituitary tumour called adenoma2
What is small for gestational age?
Gestational age means how long your mother was pregnant with you before you were born. Small for gestational age (SGA) describes children who are born smaller than usual in terms of height and/or weight, for the amount of time you were in your mother’s tummy for. Most children born SGA will catch up to other children by age 2. Children who don’t catch up by 4 years of age or later can be treated with growth hormone therapy.3
What is Prader-Willi syndrome?
Prader-Willi syndrome (PWS) is a rare genetic condition. Our genes make us who we are. This syndrome occurs when certain gene codes change or are missing. Signs of PWS may include: being very short, always feeling hungry and becoming overweight as a result, and breathing difficulty during sleep (also called sleep apnoea). Growth hormone treatment can help many children diagnosed with PWS.4
What is Turner syndrome?
Turner syndrome (TS) only affects girls. All girls have two X chromosomes, or “XX”. This condition happens if there isn’t enough or any of the second X chromosome. A common feature of TS is being very short, but other signs include heart defects, puffy hands and feet and kidney problems. Growth hormone therapy can help many children with TS grow more and reach a taller final height.5
What is chronic renal insufficiency?
Chronic renal insufficiency (CRI) means that your kidneys work less well over time. Many diseases and conditions can damage the kidneys, including autoimmune disorders, birth defects of the kidneys and other kidney disorders. Kidney problems resulting in CRI may cause ion imbalances in the blood, bone disease and loss of appetite, all of which can lead to poor growth in children. Treatment with growth hormone can help children with CRI reach a height in line with their age group.6
How are these conditions treated?
All of these conditions can be treated with growth hormone injections, which increase the levels of growth hormone in the body.3 Even though growth hormone injections can help you to grow, remember that growth is a slow process. It may take months to notice a change in height.
How does growth hormone therapy work?
Growth hormone treatment works by increasing the amount of growth hormone in the body, helping bones to grow and muscles to develop.5
What else can I do to take care of myself?
Make sure you get lots of exercise. Run, walk, dance, play sports, just have fun! Just remember that it’s also important for you to rest if you are tired.8
References
- Kato Y, et al. Internal Medicine.2002;41:1:7–13.
- Stockholm, K et al. Eur J Endocrinol. 2006;155(1):61–71.
- Sandoz. Growth hormone summary of product characteristics.
- Bakker ET, et al. J Clin Endocrinol Metab. 2013;98:4013–4022.
- Sybert VP and Macauley E. N Engl J Med. 2004;35:1227–1238.
- Hodson EM et al. Cochrane Database Syst Rev. 2012 Feb 15;2:CD003264.
- Frindik JP & Kemp SF. Biologics. 2010;4:147–155.
- Thomas SG et al. J Clin Endocrinol Metab. 2003;88:5734–5738.
All information was accessed in November 2020.